If your brain is running 37 browser tabs at once (and one of them is playing anxiety music you can’t find), guided imagery is the “close all tabs” button you actually deserve.
It’s a simple mind–body relaxation technique that uses your imagination on purpose not in a “what if everything goes wrong?” way, but in a “what if I’m sitting by a lake and my shoulders finally unclench?” way.
Guided imagery is widely used in health settings because it’s low-cost, portable, and surprisingly powerful for calming stress in the moment.
You don’t need a yoga mat, a scented candle, or the ability to “empty your mind” (honestly, who can?).
You need a few minutes, a willingness to try, and a scene that feels safe and soothing to you.
What guided imagery is (and what it isn’t)
Guided imagery (sometimes called guided visualization) is a relaxation method where you intentionally picture a calming scene or experience, often with prompts that help you engage your senses.
The “guided” part can come from an audio recording, a clinician, a therapist, or your own internal script.
The goal is a relaxed, focused state not perfection, not instant enlightenment, and definitely not “never feeling stress again.”
It’s not just daydreaming
Daydreaming wanders. Guided imagery directs.
Instead of letting your thoughts sprint laps around your worst-case scenario track, you lead them into a specific, peaceful place and keep bringing them back when they drift.
That gentle redirect is part of the magic: it trains attention the same way reps train muscles.
It’s also not hypnosis (for most people)
Guided imagery is related to other mind–body approaches and can overlap with hypnosis in some contexts, but you’re typically awake, aware, and in control.
If you try an audio recording and your mind says, “This is silly,” congratulations you’re still in charge.
Guided imagery works even when your inner narrator is a little sarcastic.
Why guided imagery relaxes you: the brain-body “switch”
Stress isn’t only a feeling it’s a full-body event.
When you’re stressed, your body can shift into a state of alert: faster breathing, muscle tension, a busy mind, and that subtle sense that everything is urgent (even when it’s just an email).
Guided imagery helps you shift out of that gear by changing what your attention is doing and how your body responds.
1) Attention moves away from threat
One reason guided imagery can feel calming is that it redirects attention away from intrusive, stressful thoughts toward a neutral or soothing mental “target.”
Many guided imagery exercises intentionally use distraction and refocusing to reduce mental noise.
You’re not ignoring your problems forever you’re giving your nervous system a break so you can return with a clearer head.
2) Sensory detail tells your body “we’re safe right now”
The biggest upgrade you can make to guided imagery is adding sensory detail.
Instead of a vague “beach,” try: the sound of small waves, warm sand under your heels, a salty breeze, sunlight on your face, the faint smell of sunscreen.
The more specific and multi-sensory the scene, the easier it is to feel absorbed and absorption is calming.
3) It supports the relaxation response
Guided imagery is commonly grouped with relaxation techniques that help the body move into a calmer state: slower breathing, reduced tension, and a steadier heart rate.
Think of it as sending your body a memo that says, “Emergency meeting canceled.”
Many people combine imagery with slow breathing or progressive muscle relaxation for an even stronger effect.
4) It reshapes your inner soundtrack
Stress often comes with mental commentary: “I can’t handle this,” “This is going to be terrible,” “I’m behind.”
Guided imagery quietly replaces that soundtrack with a different storyline: safety, ease, competence, recovery.
Even a few minutes of a calmer narrative can change how you feel and what you do next.
What the research and clinical use suggest
Guided imagery is used in many clinical and wellness settings because it can reduce perceived stress and promote calm, especially in situations like medical procedures, pain management, and anxiety-heavy moments.
Hospitals and integrative health programs often offer guided imagery recordings for sleep, relaxation, and stress coping.
Stress and anxiety support
A common use is lowering situational anxiety the kind that spikes before a procedure, a difficult conversation, or a big presentation.
Studies and reviews have reported benefits for anxiety in certain contexts (for example, perioperative anxiety), and many health systems teach it as a practical coping tool.
It’s not a replacement for therapy or medical care, but it can be a helpful skill in your toolkit.
Pain, tension, and “my body won’t unclench” days
Stress and pain can amplify each other.
When your body is braced, pain can feel louder; when pain is loud, your body braces more.
Guided imagery can help interrupt that loop by reducing stress arousal and helping muscles soften especially when paired with breathing or progressive muscle relaxation.
Sleep and winding down
Guided imagery is popular at bedtime because it gives your mind something gentle to do instead of replaying the day’s highlights (and by “highlights,” we mean mistakes from 2017).
Many people find that a short imagery track becomes a cue: “This is the part where we stop solving problems.”
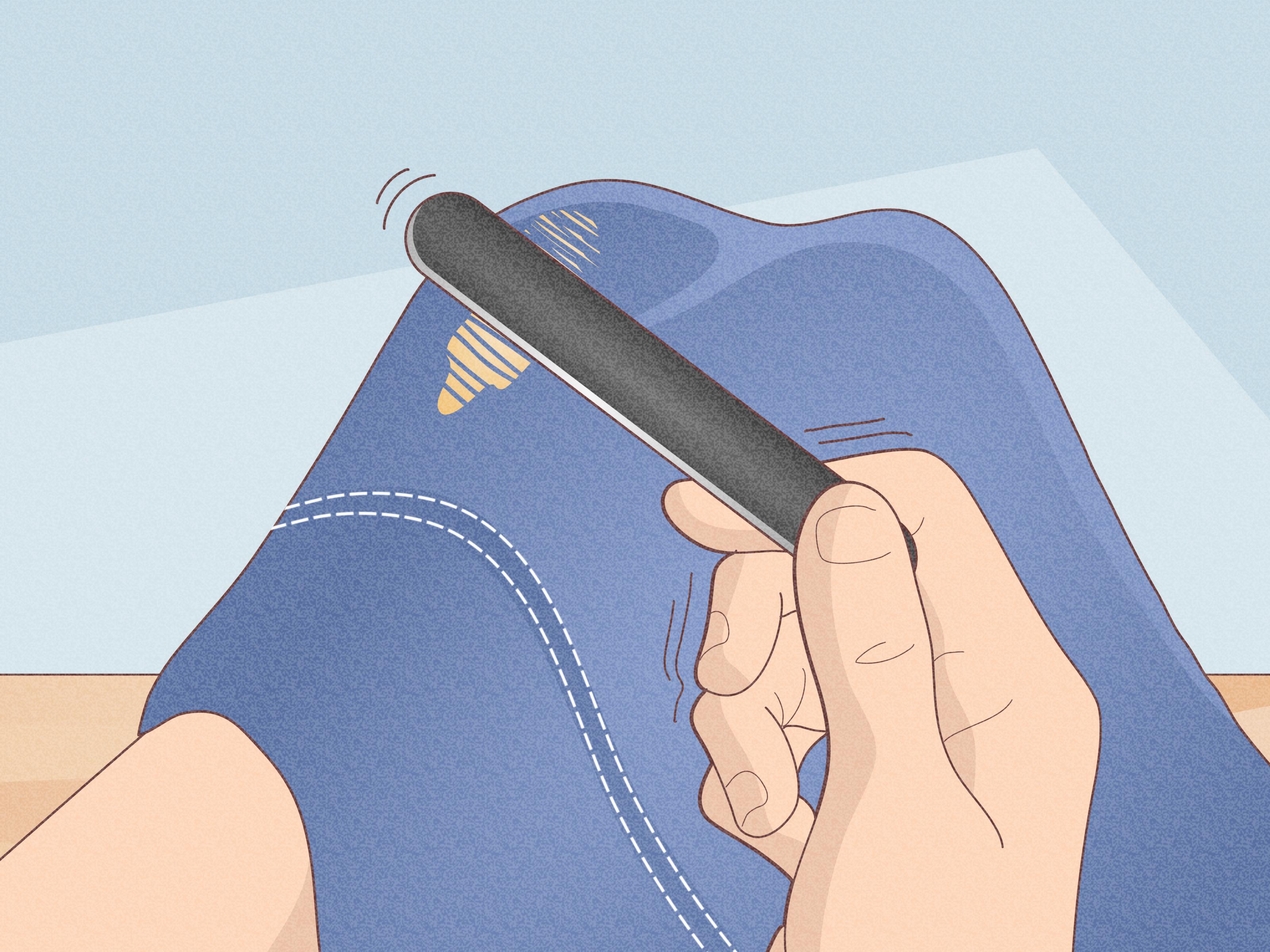
How to do guided imagery (two practical options)
You can do guided imagery with an audio recording or with a simple DIY script.
Either way, the structure is basically the same: settle your body, slow your breath, enter a calming scene, engage your senses, and return gently.
Option A: A quick DIY guided imagery routine (5–7 minutes)
-
Get comfortable.
Sit or lie down. If closing your eyes feels uncomfortable, soften your gaze instead. -
Take 3 slow breaths.
Inhale through your nose, exhale longer than you inhale. Let your shoulders drop on the exhale. -
Pick a “safe place” scene.
Choose somewhere soothing: a quiet room, a forest path, a porch in the rain, a beach, a library (yes, that counts). -
Add sensory details.
What do you see? Hear? Smell? Feel on your skin? What’s the temperature like? -
Anchor it with a phrase.
Try: “Right now, I’m safe.” or “In this moment, I can soften.” -
Return gradually.
Notice your breath again. Wiggle fingers and toes. Open your eyes and re-enter the room slowly.
Option B: Use an audio recording (the “let someone else drive” method)
Many major health organizations and medical centers offer guided imagery audio.
If your mind resists self-guided practice (“Wait, am I doing it right?”), recordings can help because you simply follow along.
Try different voices and styles you’re looking for “comforting,” not “dramatic movie trailer.”
Three guided imagery scripts you can try today
These are original examples you can read to yourself slowly or record in your own voice.
If a scene doesn’t fit, swap it out guided imagery works best when it feels personally safe and pleasant.
1) The 60-second desk reset
Sit back and let your hands rest. Take one slow breath in, then a longer breath out.
Imagine you’re stepping into a quiet elevator that only goes one floor: from “amped up” to “steady.”
As the doors close, your shoulders drop a fraction. Your jaw unclenches.
The elevator descends smoothly. With each exhale, your body gets the message: not urgent.
When the doors open, you step out into a calmer version of this same moment.
2) The “warm light” relaxation scan (5 minutes)
Breathe in gently. Breathe out slowly.
Picture a warm, comfortable light above your head like late afternoon sun, soft and steady.
As you exhale, the light drifts down to your forehead, smoothing it.
It moves to your eyes, letting them rest. To your jaw, loosening it.
Down your neck and shoulders, melting tension like butter on toast.
It travels down your arms to your hands, down your chest and belly, and through your hips and legs.
Wherever the light goes, muscles soften. Your breath stays slow. Your body becomes heavier in the best way.
3) The “favorite place” sensory scene (7–10 minutes)
Choose a place that feels peaceful. It can be real or imagined.
Notice what’s in front of you. Colors, shapes, distance.
Listen: maybe birds, a fan, wind in trees, waves, rain, or quiet.
Feel the air on your skin. Notice temperature. Notice the support under your body.
In this place, you don’t have to fix anything. You only have to be here.
When your mind wanders, gently return to one sense sound, touch, or breath and re-enter the scene.
Making guided imagery work for different minds
If you “can’t visualize,” you’re not broken
Some people don’t form clear mental pictures, and that’s more common than you might think.
The workaround is simple: use other senses or a “knowing” style.
Instead of seeing a beach, focus on the feeling of warmth, the sound of water, or the idea of open space.
You can also imagine words, music, textures, or a comforting memory without a movie-like image.
If you have intrusive thoughts
Guided imagery can be harder when intrusive thoughts interrupt.
That doesn’t mean it isn’t for you it means you need a gentle strategy.
Keep the scene simple, use a short anchor phrase, and return to a single sensory detail (like the sound of waves or the feeling of a blanket).
If intrusive thoughts are intense or persistent, guided imagery can still be useful, but pairing it with professional support may work better.
If you have trauma triggers
For some people, closing the eyes or entering certain scenes can feel unsafe.
Try imagery with eyes open, choose neutral settings (a well-lit room, a calm street, a cozy chair), and keep practice brief.
If imagery brings up distressing memories, stop the exercise and consider working with a qualified therapist who can tailor the approach.
Guided imagery vs. other relaxation techniques
Guided imagery is “mind-forward,” while techniques like progressive muscle relaxation (PMR) are “body-forward.”
Both can reduce stress they just take different routes.
If you’re the type who relaxes by stretching and releasing tension, PMR may be your gateway.
If your mind revs first and your body follows, guided imagery may be your shortcut.
The best combo: imagery + breathing
Slow breathing sets the pace, imagery sets the direction.
Try inhaling for a count of four and exhaling for a count of six while you imagine your scene.
If counting stresses you out, skip the numbers and simply make the exhale longer.
Common mistakes (and easy fixes)
-
Mistake: Trying to force calm immediately.
Fix: Aim for “10% calmer,” not “instant bliss.” -
Mistake: Choosing someone else’s perfect scene.
Fix: Pick what feels good to you (yes, even a quiet bookstore). -
Mistake: Keeping the scene vague.
Fix: Add sensory detail sound, texture, temperature, scent. -
Mistake: Quitting because your mind wandered.
Fix: Wandering is normal. Returning is the practice.
Conclusion: a calm skill you can actually keep
Guided imagery helps you relax by giving your attention a safe place to land, engaging your senses, and supporting your body’s shift into a calmer state.
It’s practical, flexible, and easy to personalize.
Start small: one minute at your desk, five minutes before bed, or an audio track when your day feels too loud.
You’re not trying to erase stress you’re learning to turn the volume down on command.
Experiences: What guided imagery feels like in real life (about )
The stories below are composite experiences realistic examples based on common ways people describe using guided imagery in everyday life.
They’re not medical claims or guarantees, but they show how this technique can fit into messy, modern schedules (and imperfect human brains).
Experience 1: The “pre-presentation spiral” becomes a reset
Jordan has a big presentation at 2:00 p.m. and a nervous system that thinks it’s about to be chased by a bear at 1:45.
Palms sweat, thoughts race, and suddenly every slide looks like it was written in ancient code.
Instead of rereading the deck for the 12th time, Jordan puts in earbuds and does a five-minute guided imagery track: a quiet path in the woods, sunlight through leaves, steady footsteps, slow breathing.
The anxiety doesn’t vanish like magic, but it stops multiplying.
By minute four, Jordan notices something small but important: shoulders drop, jaw loosens, and the “I’m doomed” feeling becomes “I’m nervous, but I can do this.”
Jordan walks into the room calmer not perfectly calm, but more present and that’s enough to speak clearly and stay on track.
Experience 2: Bedtime goes from “brain meeting” to “lights out”
Mia gets into bed and immediately remembers: an awkward text, tomorrow’s to-do list, that one comment from a coworker, and the fact that the world is full of headlines.
Sleep feels far away.
Mia tries guided imagery with a “cozy cabin in winter” scene: a warm blanket, a crackling fire, a mug of tea, snow falling quietly outside.
At first, the mind interrupts “This is corny” but Mia keeps returning to one sensory detail: the sound of the fire and the warmth in her hands.
The scene becomes a cue that it’s time to stop problem-solving.
Over a few nights, the routine starts working faster.
Mia still has occasional restless nights, but guided imagery becomes a reliable off-ramp from rumination.
Experience 3: Chronic tension gets a “soften signal”
Sam carries stress physically: neck tight, shoulders high, stomach clenched like it’s guarding secrets.
After work, Sam tries a guided imagery body-light scan.
The first week, the tension doesn’t disappear but Sam becomes better at noticing where it lives.
By focusing on warmth moving through the shoulders and down the arms, Sam starts releasing tension in small waves instead of waiting for a vacation to feel human again.
The biggest change is behavioral: Sam catches the clench earlier.
A two-minute imagery reset between tasks prevents the end-of-day crash.
It doesn’t replace stretching or medical care, but it gives Sam a skill: a way to ask the body to soften, on purpose, before stress hardens into pain.
Experience 4: Caregiver stress finds a pocket of quiet
Priya is caring for a family member and feels like “relax” is a word meant for other people.
Time is tight, emotions are heavy, and guilt shows up whenever Priya tries to rest.
Guided imagery becomes a tiny boundary: three minutes in the car before walking into the house.
Priya chooses a neutral, safe scene sitting on a porch while rain taps gently, breathing slowly, hands resting on knees.
The goal isn’t to feel happy; it’s to feel steady.
After a week, Priya notices the benefit isn’t dramatic it’s functional.
Those three minutes reduce irritability, improve patience, and make it easier to respond rather than react.
It’s a small ritual that says, “I matter too,” without requiring an hour of free time that doesn’t exist.