Electronic Medical Records (EMRs) were supposed to make healthcare safer, smarter, and more efficient. And in many ways, they have. But alongside streamlined charting and instant access to patient data came a flood of pop-ups, alerts, reminders, and warningssome helpful, some mildly annoying, and others so frequent they’ve become background noise.
This raises a criticaland increasingly debatedquestion: who do intense EMR warnings really help? Patients? Doctors? Hospitals? Or mostly the lawyers and regulators hovering in the background?
Let’s unpack the purpose, evolution, and unintended consequences of EMR warning intensity, and examine whether the system is truly serving patient safetyor simply checking boxes.
What Are EMR Warnings, Really?
EMR warnings are automated alerts built into electronic health record systems. They exist to flag potential risks, guide clinical decisions, and prevent errors before they happen.
Common Types of EMR Alerts
- Drug–drug interaction warnings
- Allergy alerts
- Duplicate test notifications
- Preventive care reminders
- Clinical decision support prompts
In theory, these alerts act like a digital safety net. In practice? That net can feel less like protection and more like a tangled mess.
The Original Promise: Patient Safety First
EMR warnings were largely inspired by landmark patient safety research from the late 1990s and early 2000s, which highlighted how medical errors contributed to tens of thousands of preventable deaths each year.
Healthcare leaders believed technology could help catch mistakes humans naturally makefatigue, distraction, incomplete information. Alerts were designed to:
- Prevent prescribing errors
- Reduce adverse drug events
- Standardize care based on evidence
- Improve compliance with guidelines
On paper, it was a slam dunk. And in certain high-risk scenarios, it still is.
Alert Fatigue: When Safety Tools Become Noise
Here’s where things get complicated.
Studies from major U.S. medical institutions show clinicians may override 60–90% of EMR alerts. Not because they’re reckless, but because many alerts are irrelevant, redundant, or clinically insignificant.
What Is Alert Fatigue?
Alert fatigue occurs when users are exposed to so many warnings that they become desensitizedeven to important ones.
It’s the digital equivalent of a car alarm that goes off every time a leaf falls on the hood. Eventually, no one looks.
Why Intensity Backfires
- Critical alerts look the same as trivial ones
- Clinicians lose trust in the system
- Workflow is interrupted repeatedly
- Decision-making becomes slower, not safer
Ironically, overly intense EMR warnings can increase risk by training clinicians to click past alerts reflexively.
Who Benefits Most From Intense EMR Warnings?
The answer isn’t as patient-centered as you might hope.
1. Health Systems and Administrators
From a compliance standpoint, dense warning systems are attractive. They demonstrate adherence to regulations, quality metrics, and accreditation standards.
If something goes wrong, administrators can say: “The system warned the provider.”
2. Legal and Risk Management Teams
EMR warnings create a digital paper trail. That trail can shift liability from institutions to individual clinicians.
In malpractice cases, the presence of an ignored alert often matters more than whether the alert was reasonable in the first place.
3. Regulators and Policy Makers
More alerts can look like more safety, even when outcomes don’t support that conclusion.
Counting alerts is easier than measuring nuanced improvements in clinical judgment.
Do Patients Actually Benefit?
The answer is: sometimes.
High-value alertssuch as severe allergy warnings or dangerous drug interactionsclearly save lives. No debate there.
The problem isn’t that EMR warnings exist. It’s that many systems treat all alerts as equally important.
High-Value vs. Low-Value Alerts
- High-value: Life-threatening interactions, critical lab values, contraindications
- Low-value: Mild interactions, theoretical risks, duplicative reminders
When intensity isn’t calibrated, patients may actually be less protectednot more.
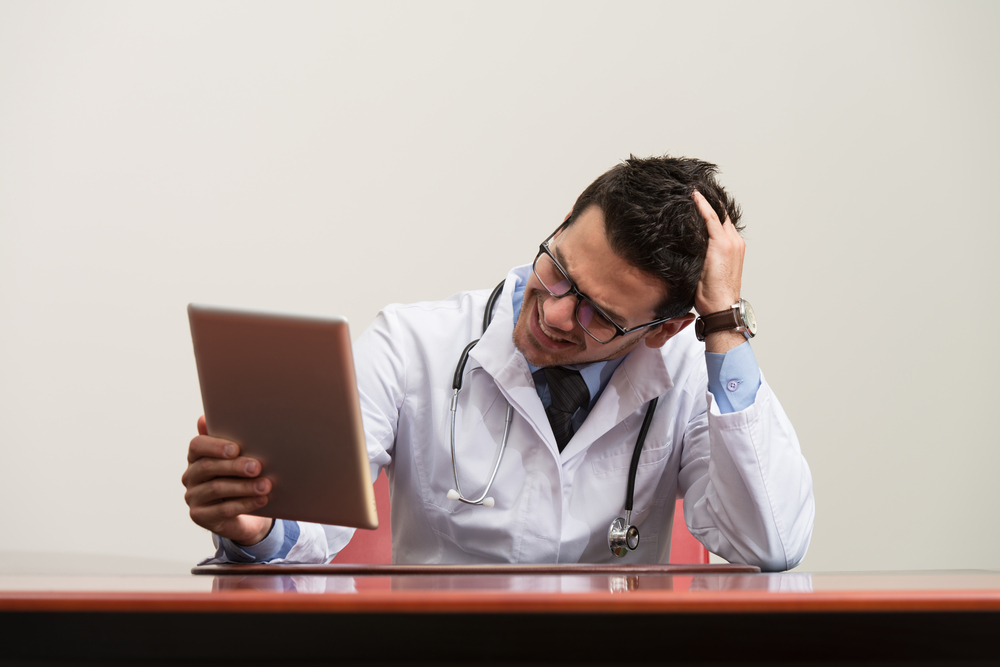
The Clinician Perspective: Between Safety and Sanity
Doctors, nurses, and pharmacists often describe EMR warnings as “death by pop-up.”
Every alert requires a cognitive decision. Multiply that by hundreds per shift, and the mental load becomes enormous.
The Cost to Clinical Judgment
Excessive alerts can:
- Undermine professional expertise
- Create checkbox medicine
- Shift focus from patient to screen
Many clinicians argue that EMR warning systems are built for worst-case scenarios, not real-world medicine.
Can EMR Warnings Be Smarter?
Yesand some systems are moving in that direction.
What Better EMR Alerts Look Like
- Tiered alerts based on severity
- Customization by specialty
- Learning systems that reduce false positives
- Clear explanations, not just warnings
The future isn’t fewer alertsit’s better ones.
Transparency Matters More Than Volume
A single, well-designed alert with context can outperform ten aggressive pop-ups.
Clinicians don’t need to be scared into compliance. They need information that respects their training and the complexity of medical decision-making.
The goal should be collaboration between human expertise and digital toolsnot dominance by either side.
Real-World Experiences With EMR Warning Intensity (Extended Discussion)
Talk to any clinician who’s worked in a modern U.S. hospital, and you’ll hear similar storiesequal parts comedy, frustration, and concern.
One emergency physician described clicking through over 200 alerts in a single 12-hour shift. Many warned about mild drug interactions irrelevant to the acute trauma cases being treated. By hour eight, the alerts stopped registering as meaningful information and became obstacles to overcome.
Nurses often share how repetitive warnings slow down time-sensitive care. A medication administration alert that requires multiple confirmations might technically improve documentation, but in practice it can delay treatment for patients in pain or distress.
Pharmacists, too, face the alert overload dilemma. While pharmacy-based EMR warnings are critical for catching true prescribing errors, many pharmacists report overriding the majority of alerts just to get through verification queues. The risk? That the one truly dangerous alert blends in with the noise.
Patients notice the effects, even if they never see the screen. Longer visits, delayed discharges, and clinicians distracted by computers rather than conversations all tie backat least in partto alert-heavy systems.
Interestingly, some healthcare organizations that reduced alert volume saw improved safety outcomes. By stripping out low-value warnings, clinicians paid closer attention to the alerts that remained. The system earned back trust.
There’s also an emotional toll. Constant warnings can subtly communicate distrustsuggesting the clinician would make unsafe choices without a machine’s intervention. Over time, that erodes morale and contributes to burnout, which itself is a patient safety issue.
On the flip side, when EMR warnings are thoughtfully designed, clinicians often become strong advocates for them. Alerts that fire rarely but matter deeply are respected. They feel like a colleague speaking upnot a manager hovering.
Ultimately, the lived experience shows that intensity alone doesn’t equal protection. Precision does.
Conclusion: Rethinking the Purpose of EMR Warnings
EMR warnings were built to help patientsbut their current intensity often serves systems, compliance metrics, and liability concerns more than frontline care.
The solution isn’t ripping alerts out. It’s refining them. When warnings are meaningful, contextual, and restrained, everyone wins: patients get safer care, clinicians regain focus, and health systems achieve realnot performativequality.
In healthcare, louder doesn’t mean better. Smarter does.